World Cancer Day 2017
KANKER LIMFOMIA (KELENJAR GETAH BENING)
PUBLIC EDUCATION
Deteksi Dini Kanker Uteri
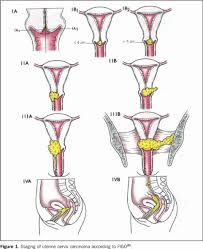 Telah kita diketahui bahwa pencegahan efektif kanker serviks merupakan tindakan preventif sekunder, yaitu deteksi lesi prakanker melalui tes Pap dan rangkaian tindak lanjut, misalnya pemeriksaan kolposkopi, biopsi. Pengalaman di negara maju menunjukkan bahwa konsep tersebut baru efektif jika cakupan populasi yang diperiksa tes Pap mencapai sebagian besar populasi yang berisiko. Namun, implementasi hal tersebut membutuhkan tidak hanya biaya, melainkan juga sumber daya manusia dan logistik peralatan yang besar.
Telah kita diketahui bahwa pencegahan efektif kanker serviks merupakan tindakan preventif sekunder, yaitu deteksi lesi prakanker melalui tes Pap dan rangkaian tindak lanjut, misalnya pemeriksaan kolposkopi, biopsi. Pengalaman di negara maju menunjukkan bahwa konsep tersebut baru efektif jika cakupan populasi yang diperiksa tes Pap mencapai sebagian besar populasi yang berisiko. Namun, implementasi hal tersebut membutuhkan tidak hanya biaya, melainkan juga sumber daya manusia dan logistik peralatan yang besar.
Gawat Darurat dibidang Kanker
 Kedaruratan Kanker (Oncologic Emergencies) didefinisikan sebagai kejadian akut, yang berpotensi mengancam nyawa, baik secara langsung maupun tidak langsung berhubungan dengan kanker atau pengobatan kanker. Gawat darurat kanker bisa timbul dari kemampuan kanker untuk menyebar, serta menginvasi struktur disekitarnya dan metastasis pada tempat yang jauh.
Kedaruratan Kanker (Oncologic Emergencies) didefinisikan sebagai kejadian akut, yang berpotensi mengancam nyawa, baik secara langsung maupun tidak langsung berhubungan dengan kanker atau pengobatan kanker. Gawat darurat kanker bisa timbul dari kemampuan kanker untuk menyebar, serta menginvasi struktur disekitarnya dan metastasis pada tempat yang jauh.